Brown recluse spider, Violin spider
Brown recluse spider, Violin spider |
This spider is found in many parts of the U.S.A. and has extended its range to the northern states. It often hides under stones and in dark corners inside buildings. It has a leg span of about 2.5 cm (1 inch) and a peculiar violin-shaped design of the back. Its venom may cause severe mechanical damage expressed in necrotic lesions. It destroys the walls of blood vessels causing nasty skin ulcers that take long to cure. Fatal bites are rare.
Introduction
The devastation caused by the bite of the Brown Recluse spider can be stopped in its tracks and reversed, even at advanced stages of its degenerative effects.
The Recluse bite can cause a prolonged and expensive trail of suffering and disability to its victims. The frequency of bites to humans has increased at an alarming rate, as the spider moves indoors and into our garments, shoes and bedding. Treatment cost now run into the millions of dollars per year and are rising rapidly as incidences increase.While some spiders inject little venom, others may be expected to create serious management problems with resultant extensive tissue loss, pain. disability and chronic deterioration.
The etiology is the powerful, vasoconstricting properties of the venom, as the mechanism of necrotic arachnidism, which causes the smail arteries to spasm with resultant loss of blood supply to the bite area. This sets up a cycle of ulceration and tissue loss through ischemia and gangrene. Systemic medication alone is unable to penetrate the lesion because of the barrier zone produced by the spastic occlusion of the arteries.
However...a nitroglycerin patch can penetrate through the skin, into the interstitial fluid and into the capillaries, rapidly dilating the vessels. This is evidenced by the quick onset of a nitroglycerin headache as circulation into the occluded area is re-established from the edges inward. The pathologic process ceases and healing begins. When a nitro patch is administered early, as in the first 48 hours, no lesion ever develops! Delay treatment three to four weeks and a 5 cm ulcer will develop, requiring three months of treatment with the nitroglycerin patches. Even with delayed treatment, however, the degenerative process is reversed. The body heals itself. There is no need for surgery with its debilitating effects, potential complications and severe scarring.
The patch is cut to cover only the effected area, right up to and extending just over the edge of involvement. In the case of a youngchild, the patch should be cut down to cover the smallest area possible, with more frequent removal and reapplication necessary. Pictures of the recluse bites treated with these patches provide examples of some responses.
With few exceptions, regardless of the site of the bite or the age and health of the patient, the patch has stopped the progress of the tissue loss, thus allowing the area to begin recovery, usually without scarring and with only slightly darker pigmentation.
 |  |
 Exceptions include a patient with a very old ulcer (10 months), one whose bite was at the posterior knee joint and who was not diligent in keeping the patch on in this difficult location, and a patient whose auto immunity was compromised by HIV. I have found the Deponit Nitroglycerinpatch to be the most effective patch of the several types tried because the nitroglycerin is dispersed throughout the matrix, the dosage is easily controlled, and the patch is very flexible (important for joint areas). Nitroglycerin spray was also used, and found to be very effective when applied to a bite of no more than several days age. Under no circumstances will oral nitroglycerin be appropriate. With blood flow re-established to the bite site, systemic antibiotics are effective and patients are prescribed Ciproflaxin for the first five to seven days to counteract bacteria - possibly delivered by the spiderâs fangs - and to prevent potential bone involvement. Patients should be instructed that in the event of a headache the patch should be removed for up to one hour and then replaced.
Exceptions include a patient with a very old ulcer (10 months), one whose bite was at the posterior knee joint and who was not diligent in keeping the patch on in this difficult location, and a patient whose auto immunity was compromised by HIV. I have found the Deponit Nitroglycerinpatch to be the most effective patch of the several types tried because the nitroglycerin is dispersed throughout the matrix, the dosage is easily controlled, and the patch is very flexible (important for joint areas). Nitroglycerin spray was also used, and found to be very effective when applied to a bite of no more than several days age. Under no circumstances will oral nitroglycerin be appropriate. With blood flow re-established to the bite site, systemic antibiotics are effective and patients are prescribed Ciproflaxin for the first five to seven days to counteract bacteria - possibly delivered by the spiderâs fangs - and to prevent potential bone involvement. Patients should be instructed that in the event of a headache the patch should be removed for up to one hour and then replaced.
I have been using this procedure in my private practice since 1989 with amazing and conclusive results. In instances where I see the bite so early on as to be unable to positively identify as a Brown Recluse bite (most times the victim does not see the spider, or if they do the response is to pulverize it, thus allowing no method of identification other than an examination of the affected area), I will initiate treatment with the nitroglycerin patches as a precaution. There is no danger from its use on other bites, but to delay treatment from uncertainty only allows further degradation and necessitates a prolonged treatment period. The patch will also help scorpion and other bites anyway. Exception: Do not use on snake bite.
Current Methodologies
Excluding nitroglycerin patches, the most widely used treatment methodologies have all proven to be ineffective. Treatments such as ice packs, oxygen pressure chambers, surgery, systemic medications and too many more to list here have all provided such inconsistent results, prolonged treatment duration and high cost as to be very questionable for any continued usage. The nitro patch is the only therapy that is effective as of now. It is simple, inexpensive and effective beyond belief.
Symptoms
Rarely does the patient know they have been bitten by a spider, as the bite is painless. The patient notices later that they have been bitten by something. It may look as innocuous as a mosquito bite! However, they soon notice the changing appearance of the lesion and the malaise, fever and flu-like symptoms that often occur from 4-8 hours after the bite. If untreated by the nitroglycerin patch there soon forms a series of ulcerations and debridements of
varying degrees. Surgical Excisions could span up to 18 months. This is followed by residual disability that is often of a major nature, such as chronic weakness, an inability to stand for extended periods, recurring
migraine headaches, loss of limb and even death.
Identifying The Bite
There are several characteristics to look for. They may not all be present and will vary in their clarity. However, if you look at a couple of pictures and see a few bites, identification becomes easy.
The basic visual characteristic is a central small bulls eye effect with the next ring being white and the outer ring being red.
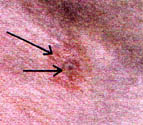 |
A new bite will have a small, central hole that looks like a deep, dilated skin pore, as if a tiny drill was used.
 |  |
The hole will fill with a black, necrotic tissue that looks like a small pencil lead. This drains out and will swell closed. A blackish, larger bulls eye develops, which turns red as the outer red zone finally turns the entire lesion red.
 |
Approximately 10% of the time, you will see small, cut-like fang marks that may turn black and gangrenous within a few days. This area is the gangrenous zone and will finally take over the entire lesion in a few weeks, becoming a grayish-red.
 |
The original second circle may be the size of a dime or larger in a bigger lesion. As it grows, if you look closely, you can usually see the perfectly circular area of paler tissue. This is the zone of ischemia, which will finally loose its battle - unless you come to the rescue with a nitroglycerin patch, actually reversing the process of degradation. The red, outer ring can encompass the entire area in four to five days. Usually, an untreated lesion will turn pale as it spreads outward and constricts the vessels, producing ischemia.
 |
Beneath the red, elevated area, the necrosis is spreading and suddenly the entire area sloughs out. (at about 3 weeks). Do not mistake this as purulent. To the contrary, this is a slough of tissue fluids and necrotic tissue.
 |
Even at this stage, using daily nitroglycerin patches that cover the entire lesion, the wound will heal as quickly as three to four months.
The wound in the picture below was totally healed in 11 weeks!! (see back page for documented pictures of the stages of healing)
 |
This is a tremendous response as opposed to twelve to eighteen months of several surgeries and skin graphs (which often do not survive), and the extensive pain and suffering of the patient. I hope you will see all lesions early enough to prevent this.
Wound Care
Should you find the wound in the advanced stages, clean the wound (lightly, do not use conventional wound care), leaving a clean ulcer. This is the only time you should clean the wound. Further cleaning will only hamper the formation of the new cellular structures being promoted by reestablished circulation. You must allow the body to heal itself in this area. Many times the red area has prevented correct assessment of the etiology of the lesion. Most times the assumption is that the red skin is due to hyperemic circulation, when actually it is due to the mast cells, etc., involving the area in an attempt to heal the lesion. Do not cut away the tissue!! I cannot emphasize this enough.
It will be incorrect. The cells, if left alone will form the specie functional tissue needed. In a new wound, the cell is told what tissue is to be replaced next to it, The reason we don’t clean the wound is that this D.N.A. map is totally distroyed leaving a nonfunctional scar tissue. (For more information on the fascinating new discoverys being made about tissue regeneration, contact me at the address on the back.)
Treatment Procedure
If in doubt to the correct diagnosis, use the nitroglycerin patch - the stakes are too high to allow a recluse bite to go untreated! As stated earlier, the patch will also help scorpion and other bites anyway. Again, as an exception, do not use on snake bites.
Use a 0.1 mgm/hr or a 0.2 mgm/hr patch. I have found this is all that is required and have almost no problems. I prefer the Deponit Nitroglycerin Transdermal patch. Cut the patch to approximately the size of the lesion, to be placed right up to the edge of the outer ring.
 |  |
This allows even small children to be treated. Change the patch daily. A new bite will disappear in one to two days. However, treat for one week as a precaution against a reoccurrence from inadequate treatment.
The average lesion requires about two or three weeks of treatment. Should one allow a lesion to ulcerate - getting 3 to 5 an in diameter - it my require 3 months of treatment. However, the patient can continue working during this treatment period!
Oral antibiotics, such as Ciprofloxin, are used for the first five to seven days to prevent the possibility of any abscess formation, secondary infection and potential bone involvement.
Do not apply topical ointments, such as Betadine, etc. No soaking in any solutions. Again, No soap and water cleaning. No debridements, etc. Leave the lesion alone. You should only dean around the wound, Use only the nitroglycerin patch. I know this may be difficult to do since we are taught to âthoroughly" dean everything. The patient should be instructed not to clean the wound and only periodically allow water to wash over the area at most and then allow to air dry prior to reapplication of the patch.
Kenneth G. Burton
References
- Acerrano A. "Along came a spider” Sports Afield 1995. 213: 22-23
- Bowles D. "Spiders, truth and fiction" Texas Parks and Wildlife 1995. 24-27
- Preston-Mafham. R.K. Spiders of the World. NY: Fats on File Publications. 1984.
- Purdy C. "The buzz of bees and stings." Current Health 2. 1992 19-26
- Morelli J. "Battling the Brown Recluse with innovation” World and l. 1994. 9: 187-189.
- Milne L.J. The Audubon Society field quote to North American Insects and Spiders. 1992. 874-876
- Kaston B.J. How to know the spiders. Third Edition. Dubuque: Wm C. Brown Co. 1972, 265pp
- Glucman S., Talley J.H. “Acute care for bite wounds; venomous spiders; Think black or brown." Patient Care. 1995. 29: 170-174
- Cooke J. "At the museum. A pioneering spider man?” Natural History NY: Museum of Natural History. 1996 103:74
- Shulman S. “Venomous pursuit." Technology Review. 1992 94: 15-16
- Smith R.L. "Poisonous plants and animals." Academic American. Danbury, conn: Golier Inc. 1996. 15: 383-385
- Kelsey A.M., Schneidermon H. "What's your diagnosis?” Consultant. 1995. 1013-1013
- JAMA “Necrotic Arachnidism-Pacific northwest 1988 - 1996" JAMA Centers for Disease Control. 1996. 275: 1870 -1871.
- Davis B.D., Dulbrcco R., Eisen H.N. et al. Microbiology incluluding immunolgy and molecular genetics. Second Edition. Hagerstown My: Harper and Row. 1973. pp: 645, 646, 851-852, 882, 899.
- Alison W.E. Jr., Shac R.B., Lynch.S. "Pyoderma Gangrenosum. A long term complication of the brown recluse spider bite." Plastic and Recponstructive Surgery.
- AAFP. "Brown recluse spider bites in pregnant women" Kansas City, No. American Family, Physician. 1992. 6: 2749
- S., Kohn M., Baker D., Vandrleest R., Gomex H., McKinney P., McGoldrick J., Brent. "Therapy of brown spider envenomation: a controlled trial of hyperbaric oxygen, dapsone, and cyproheptadine." Annals of Emergency Medicine. Ft. Collins: Colo. State School of Veterinary Medicine. 1995. 25: 363-368
- Munn G.E., Rosen T. "Management of brown recluse spider bite". Consultant. 1992. 32: 91
- Warrell D,A., Fenner P J. "Venomous bites". British Medical Bulletin. London Medicai Dept. The British
